The wall between your facility and your community
Timely access to quality healthcare services has a profound effect on every aspect of a person’s health. However, rural residents, who account for almost 19.3% of the US Population, are facing inequalities when it comes to both access and quality of healthcare.
Rural healthcare facilities are left to bear the burden of caring for these unique communities. Solutions that get carried over from urban areas are proven to be, not only ineffective, but detrimental as they fail to address the unique barriers to healthcare access of rural America.
The Five Barriers to Rural Healthcare Access:
- Workforce Shortages.
- Distance, Transportation & Internet
- Health Insurance Coverage
- Social Stigma and Privacy Issues
- Poor Health Literacy


Workforce Shortages
Less than 8% of all physicians and surgeons choose to practice in rural setting. The workforce shortages extend to all healthcare professionals from medical management to health aides and it is one of the more significant barriers to quality healthcare access. The shortages create an enormous burden to both the facilities and the communities. The facilities are facing increasing costs from constant recruiting efforts. Facilities are having difficulty maintaining quality from high turnaround and unfilled positions. More importantly, facilities lose their community’s trust.

Distance, Transportation & Internet
Geographic access is another rural healthcare access barrier. 97% of the country’s land mass is rural but only 19.3% of the population lives there. Sparsely populated areas result in longer travel distances to access healthcare. The travel burden is amplified by the road conditions, the terrain and the weather. The distance-to-provider is also affected by the ability of the rural residents to secure transportation. Socioeconomic factors limit the access to reliable private transportation and most rural communities luck adequate public transportation making accessing healthcare very difficult.
The luck of high-speed internet with a reliable connection is another factor widening the distance-to-provider. 39% of rural residents do not have access to high-speed broadband internet. This translates to an inability to research nearby healthcare facilities, plan routes and even worse, rural residents are denied access to telemedicine services that could provide a solution to the geographic limitations.

Health Insurance Coverage
9.1% of residents leaving outside metropolitan statistical areas, are without any type of health insurance. Rural residents, when compared to their urban counterparts, face higher health insurance premiums, difficulty affording their co-pays, less access to low-cost or charity healthcare as well as less providers to choose from in their participating plan. As a result, rural residents are delaying or even forgoing seeking healthcare.

Social Stigma and Privacy Issues
Anonymity, privacy and social stigma are significantly tougher barriers to overcome in rural communities. Rural residents can feel apprehensive in seeking healthcare because of lack of privacy and anonymity. Family, friends and co-workers can easily find out when a resident seeks medical attention, either due to direct observation or because they are working in the healthcare facilities themselves. The problem intensifies when rural residents are seeking care for conditions associated with social stigma such as mental health, substance abuse, sexual health, etc.

Poor Health Literacy
Rural residents have a higher risk for low health literacy, because on average, they have lower education levels, they are living in poverty or do not have English proficiency. Low health literacy not only affects the health choices an individual makes, but also their ability to understand and follow healthcare instructions or navigate the complex healthcare system.
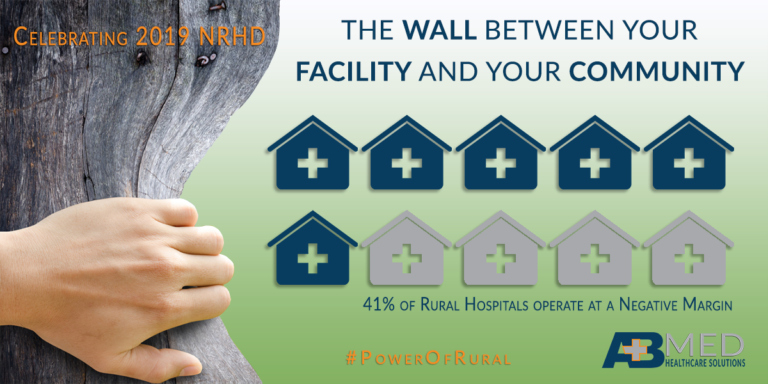
Supporting the Rural Facilities
Rural healthcare facilities are losing the battle with providing care to their communities while keeping their doors open. The new emerging barrier to healthcare access is the closure of rural facilities or the discontinuation of services. 41% of rural hospitals operate at a negative margin and 161 rural hospitals have closed since January 2005. Each time a rural facility downsizes or closes, there are severe consequences that are felt throughout the local and surrounding communities. Apart from the obvious loss of healthcare services, there is loss of jobs, loss of tax revenue, loss of supporting business and loss professional residents.
AB Med believes that the solutions need to work for both sides the facility and the community. We believe in Healthy Facilities, Healthy Communities! Contact us to learn how we can assist your facility in providing the healthcare quality that your rural community deserves! Let’s Connect.
We at AB Med are excited to talk to you, contact us
Rural Health is our passion and focus
REFERENCES & RESOURCES
- About Rural Health Care, https://www.ruralhealthweb.org/about-nrha/about-rural-health-care
- Life in the slow lane: Welcome to the internet in rural America, https://www.cnet.com/news/life-in-the-slow-lane-welcome-to-the-internet-in-rural-america/
- Healthcare Access in Rural Communities, https://www.ruralhealthinfo.org/topics/healthcare-access
- Social Determinants of Health for Rural People, https://www.ruralhealthinfo.org/topics/social-determinants-of-health#literacy-and-education
- 161 Rural Hospital Closures: January 2005 – Present (119 since 2010), https://www.shepscenter.unc.edu/programs-projects/rural-health/rural-hospital-closures/
- Access to Rural Health Care – A Literature Review and New Synthesis, http://www.rupri.org/Forms/HealthPanel_Access_August2014.pdf#page=9
- Exposing some important barriers to health care access in the rural USA, https://www.ncbi.nlm.nih.gov/pubmed/26025176
- Healthcare Access in Rural Communities, https://www.ruralhealthinfo.org/topics/healthcare-access
By: Erik McLaughlin MD, MPH and Aikaterini Papadopoulou, B.Arch






