Obesity is an issue that threatens the health of millions of Americans—but especially those that live in rural communities. As we head into 2023, it is important for healthcare leaders in these areas to understand the severity of the obesity epidemic in rural America and to develop public health programs and initiatives in response.
In this article, we will highlight the prevalence and risks of obesity in rural America as well as break down some of its contributing factors. We will also suggest ways healthcare leaders, local governments, and community stakeholders can work to alleviate this growing epidemic.
Let’s dive in.
The Obesity Epidemic
What makes obesity so serious health-wise is its interrelation with chronic disease. The CDC reports that obesity is a risk factor for “type 2 diabetes, coronary heart disease, some cancers and arthritis.” [iii]. It can also be a risk factor for high blood pressure and even certain kinds of cancer. [i]
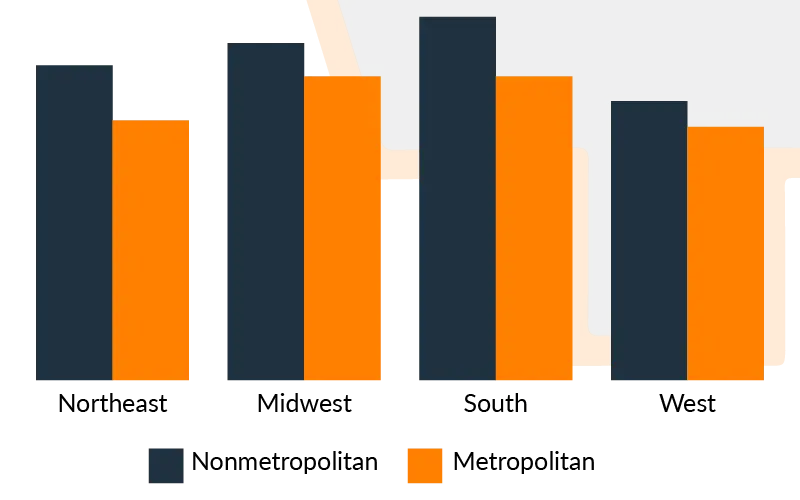
However, research has shown that this epidemic does not affect all communities equally.
The Prevalence of Obesity in Rural Communities
These findings are consistent with other public health threats; rural communities are often disproportionately affected by disease and health risks.
Why is that so?
Let’s look at some contributing factors to the obesity epidemic in rural America.
Compared to their metropolitan counterparts, rural communities often have fewer resources that can help lead to healthier lifestyles. For example, many rural communities have a shortage of healthcare specialists like nutritionists and dietitians. [iv]
In addition to these shortages of specialists, rural communities also often have limited access to healthy foods such as fresh fruits and vegetables. And even when these healthier foods are available, they can be cost-prohibitive. According to a report from the NCBI, “Many people who reside in rural communities lack facilities and resources that can enable them to adopt positive dietary practices due to their low socioeconomic status.” [v]
Another challenge these communities face, as reported by the National Rural Health Association, is “limited access to exercise facilities and infrastructure such as gyms or walking trails.” [i] Unlike in urban cities, most rural populations depend on cars—rather than walking—to get from place to place daily. And when there aren’t any exercise facilities available, prioritizing physical activity can be even more difficult.
Finally, one of the most significant issues impacting the prevalence of obesity in rural communities is access to healthcare services. Specialists aside, populations living in rural parts of the United States often must travel great distances to receive medical care. [iv] With no accessible or convenient care options available, it’s easy to see how these communities might opt to forgo healthcare services altogether.
Metropolitan vs. Nonmetropolitan Comparison
An estimated 60 million Americans live in rural parts of the U.S.—many of whom are experiencing some, if not all, of these healthcare barriers and challenges. [v] Understanding the threat of the rural obesity epidemic is only part one of the process; healthcare leaders and community stakeholders should be making coordinated efforts to minimize these challenges moving forward.
Some Solutions to the Obesity Epidemic in Rural America
By breaking barriers to care and developing different public health initiatives, public health leaders can work toward slowing the obesity epidemic in their communities.
Some rural obesity-prevention strategies recommended by the CDC include “increasing the availability of healthy food…opening public buildings (e.g., school facilities) after hours for physical activity purposes; and including bicycle paths, paved sidewalks, and outdoor public recreation facilities in community planning.” [iii]
The Rural Health Information Hub also suggests that communities can “develop programs and services that help rural residents learn about the health risks of overweight and obesity, as well as adopt healthy lifestyle behaviors to control their weight.” [iv]
Partnering to fight the obesity epidemic in rural America
If you want to start implementing some of these strategies and creating new initiatives, we can help. At AB Med, we can support rural healthcare leaders to help them break down barriers to care, address limiting social determinants of health, and develop effective and relevant programs to address the obesity epidemic.
With over 75 years of combined experience in the healthcare industry, we understand the intricacies of designing, creating, and executing innovative public health solutions. Let’s work together to minimize and alleviate the threats facing the health of rural communities in 2023 and beyond. Let’s Connect.
REFERENCES & RESOURCES
- www.ruralhealth.us . (n.d.). NRHA’s new rural obesity and chronic disease partnership – NRHA. [online] Available at: https://www.ruralhealth.us/blogs/ruralhealthvoices/october-2022/nrha-s-new-rural-obesity-and-chronic-disease-partn [Accessed 4 Jan. 2023].
- Centers for Disease Control and Prevention (2021). Adult Obesity Facts. [online] Centers for Disease Control and Prevention. Available at: https://www.cdc.gov/obesity/data/adult.html.
- CDC. (2019). CDC: More obesity in U.S. rural counties than in urban counties. [online] Available at: https://www.cdc.gov/media/releases/2018/s0614-obesity-rates.html.
- Ruralhealthinfo.org. (2014). Rural Obesity and Weight Control Introduction – Rural Health Information Hub. [online] Available at: https://www.ruralhealthinfo.org/topics/obesity-and-weight-control.
- Okobi, O.E., Ajayi, O.O., Okobi, T.J., Anaya, I.C., Fasehun, O.O., Diala, C.S., Evbayekha, E.O., Ajibowo, A.O., Olateju, I.V., Ekabua, J.J., Nkongho, M.B., Amanze, I.O., Taiwo, A., Okorare, O., Ojinnaka, U.S., Ogbeifun, O.E., Chukwuma, N., Nebuwa, E.J., Omole, J.A. and Udoete, I.O. (2021). The Burden of Obesity in the Rural Adult Population of America. Cureus, [online] 13(6). doi:10.7759/cureus.15770.
- Ruralhealthinfo.org . (2014). Rural Obesity and Weight Control Introduction – Rural Health Information Hub. [online] Available at: https://www.ruralhealthinfo.org/topics/obesity-and-weight-control.
By: Erik McLaughlin MD, MPH and Aikaterini Papadopoulou, B.Arch