2024 Update: Addressing Heart Failure Risks in Rural America
RURAL HEARTACHES 2024: Cardiovascular Disease in Rural America
In 2024, the landscape of rural cardiovascular health in America continues to evolve, revealing both persistent challenges and innovative responses. The disparity in heart health between rural and urban communities is more pronounced than ever, demanding focused attention and tailored strategies.
Elevated Heart Failure Risks in Rural Populations:
A large observational study by the National Institutes of Health has uncovered a startling 19% higher risk of heart failure in rural American adults compared to their urban counterparts, with Black men in rural areas facing a particularly high risk. This discrepancy calls for specialized approaches to heart failure prevention in these communities [1].
Collaborative Efforts to Bridge the Care Gap:
The American Heart Association, in collaboration with the National Rural Health Association and the American College of Emergency Physicians, is at the forefront of efforts to reduce cardiovascular disparities. Their initiatives include sharing crucial cardiovascular and stroke clinical resources and enhancing care in rural hospitals to deliver equitable healthcare irrespective of geographic location [2].
Addressing Cardiovascular Disease in Rural America
In the United States, the prevalence of cardiovascular disease poses a significant health concern, particularly in rural America. Every 40 seconds, an American experiences a heart attack, and cardiovascular-related incidents result in more than one death per minute. The consequences of heart attacks extend beyond immediate risks; survivors often endure long-term damage that hinders their quality of life. Rural communities face additional challenges, with conditions like heart arrhythmias, leaky valves, and cholesterol-clogged arteries posing further risks, including stroke.
The reality of cardiovascular disease in rural America is marked by limited medical resources. Quick access to medical care is crucial for survival and recovery from heart attacks, yet in these areas, healthcare services are often stretched thin. First responders provide essential initial stabilization, but the journey to advanced care involves transportation—sometimes long-distance—to larger medical centers where specialized cardiac care, including the expertise of cardiologists, is available.
Let’s talk about Rural Heartaches
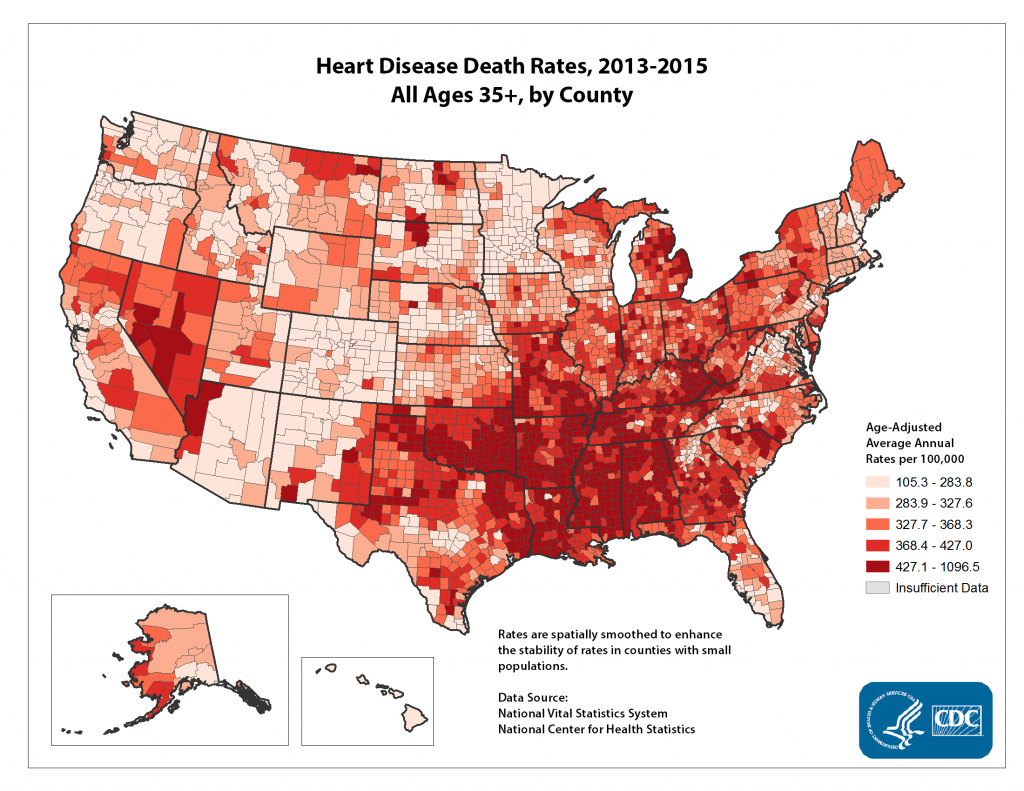
CARDIOVASCULAR DISEASE DISPARITIES
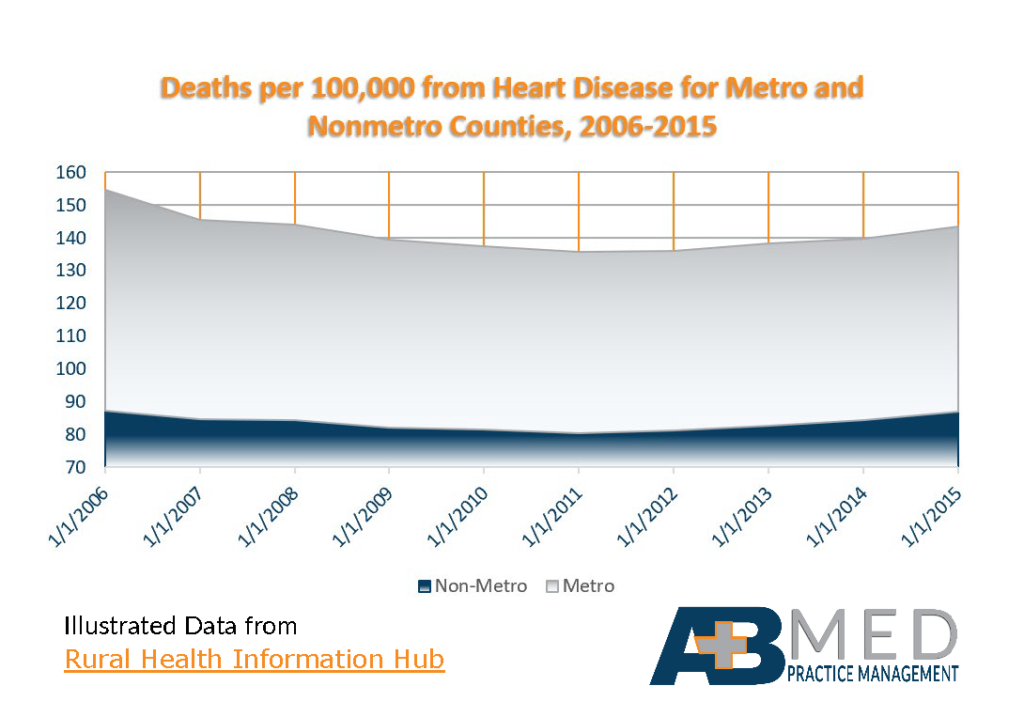
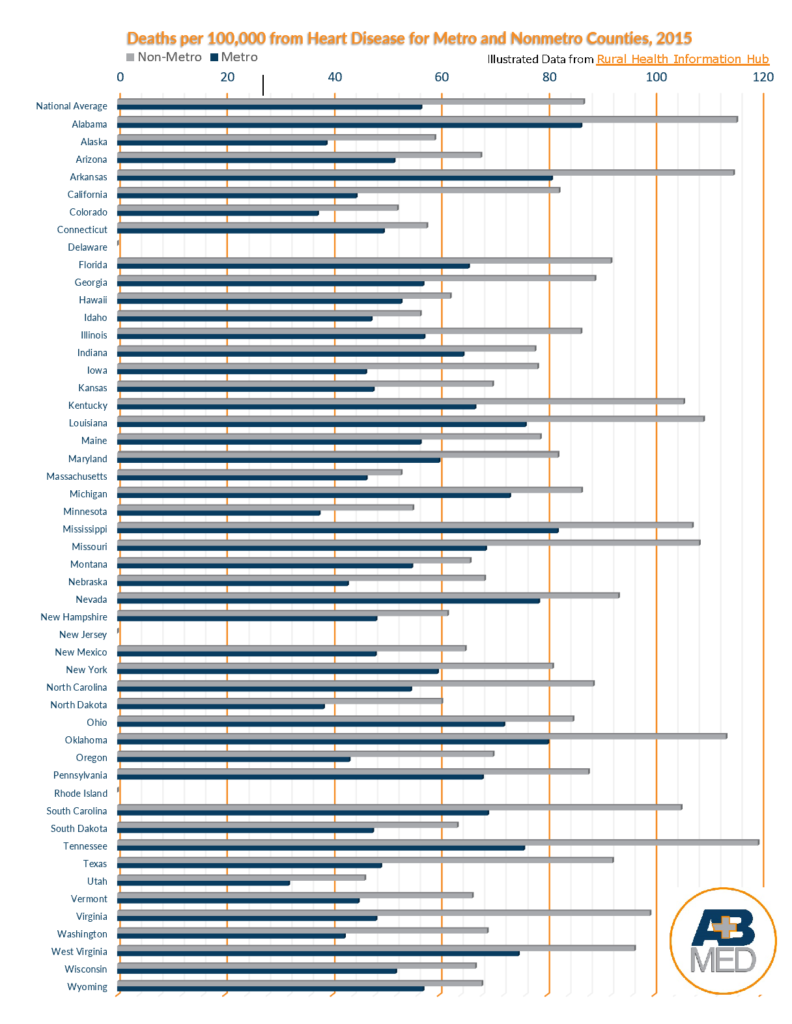
Throughout America, more people living in rural communities die from cardiovascular disease, or “CVD,” than do those living in metropolitan areas. The list below, obtained from line charts provided by the Rural Health Information Hub shows the seriousness of this disparity. The list compares, state by state, the number of deaths in 2015 from CVD per every 100,000 persons who were living in non-metro, or rural, counties to those living in metro, or urban, counties.
For the past 3 years I have held the position of Networking Chair on the Arizona Healthcare Executives’ (AHE) Programming Committee. The most profound aspect of being in this position was witnessing how small the healthcare world is and experiencing how intertwined we all are. These, usually unknown, connections span diversity, unite healthcare sectors, link healthcare settings, and transcend job responsibilities. I’ve learned how networking can open up unknown job markets, foster support, inspire encouragement, cultivate relationships, and is seen as a marketable asset.
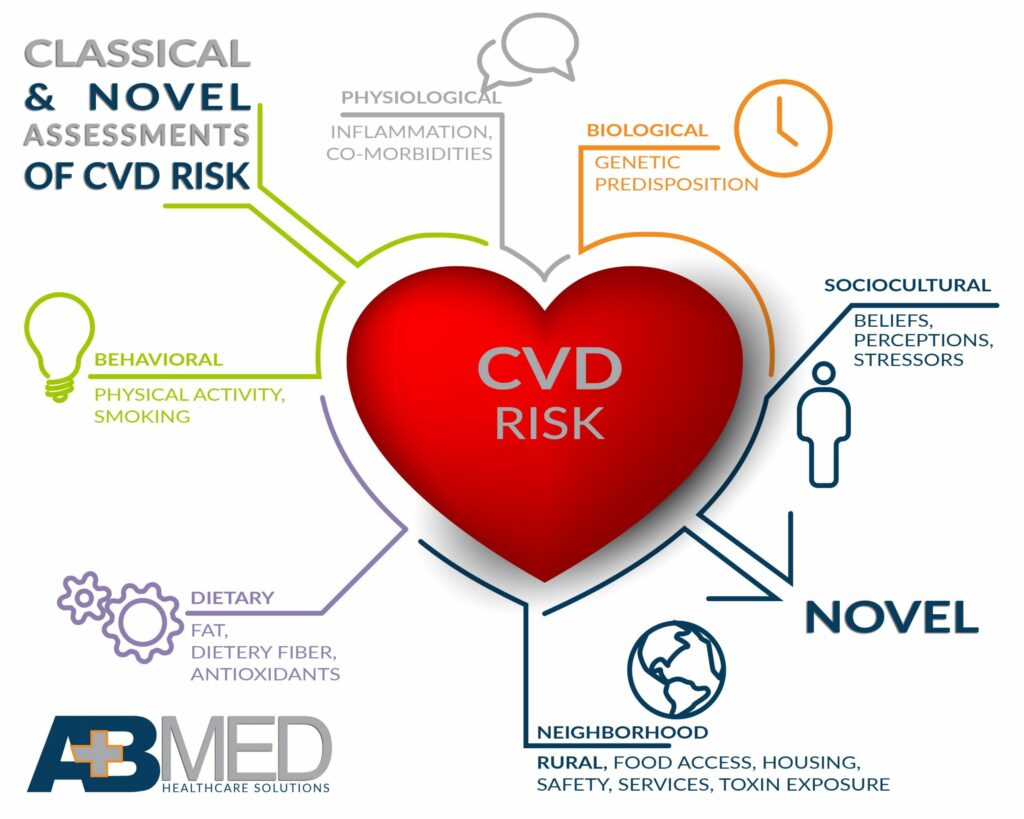
FACTORS OF CARDIOVASCULAR DISEASE DISPARITIES
The national Centers for Disease Control and Prevention, or “CDC,” published an article on February 26, 2018, entitled “Mission Possible: Addressing Health Disparities in Heart Disease and Stroke Outcomes.” The article mentions the following causes of higher rates of death that occurs in rural areas as a result of cardiovascular disease:
- Less education
- Lower incomes, reduced ability to pay for medical help
- Increased tobacco use
- Poor diet
- Lack of physical activity
- Traumatic backgrounds
- Fewer opportunities for social supports
Reducing Inequalities Requires Teamwork
Reducing such rural health disparities requires a concerted effort by members of rural communities to address the problems involved, identify and assess risk factors before serious heart problems develop, and provide outstanding rural healthcare. At AB Med Healthcare Solutions, LLC, we wholeheartedly support the efforts of rural healthcare practice management to close the gap and provide the best care possible.
Assessing cardiovascular risk factors can be tricky. First, not everyone agrees on what the risk factors are. Ones that often are assessed include diabetes, leisure-time physical inactivity, obesity, high LDL cholesterol, high blood pressure and tobacco use. Three that also might be considered are low serum levels of Vitamin D, thyroid dysfunction and untreated sleep apnea.
Classical & Novel Assessments of CVD Risk
Sometimes, patients are reluctant to provide accurate information or to undergo testing. Also, test results may not provide a complete picture, one that will give the physician the knowledge needed to take appropriate action. For example, an angiogram may show the formation of blood clots rather than an artery clogged by plaque. However, it does not reveal why the blood clots exist. Resolving the problem and reducing risk may involve prescribing medication as well as determining whether vitamin supplementation or reduction is needed. Making both classical and novel assessments of CVD risk increases the likelihood of assessment accuracy.
Medical practice management teams that take an active part to address the problems in our communities that contribute to a higher incidence of cardiovascular disease make a huge difference in the lives of community members and their families. Every heart attack prevented or life saved affects the lives of several others.
Management teams and the staff we supervise may unite with local schools, senior citizen centers and restaurants to educate the public as to the existence of locally grown foods that are healthy, ways to prepare well-balanced meals that please the taste buds, and small dietary changes that make a big difference over time. Other areas in which members of practice management have the opportunity to affect positive change include the following:
- Sponsoring events or competitions that require physical activitys
- Using social media as well as local media outlets to help increase knowledge of the risk factors for heart disease
- Presenting ways people can lessen their risks
- Publicizing the signs of a heart attack and the importance of getting help without delay
- Holding health fairs and free clinics on heart health
- Providing additional access to healthcare for those who are isolated or poverty-stricken
Providing additional access to healthcare may mean making home visits or furnishing transportation. It might involve applying for grants and researching other avenues for increased funding so that rural facilities can stay open. It also may require finding some way to keep the facility fully staffed even though qualified workers are scarce.

Healthier Rural Hearts

The staff at AB Med are here for you and your community. Whether you are struggling to hire and keep qualified staff, need help in clinical or administrative leadership, or would like the services of a public health consultant, we have the knowledge and expertise to fill your needs and help reduce disparities so that residents of your community can look forward to healthier hearts and longer lives. Let’s Connect.
We at AB Med are excited to talk to you, contact us
Rural Health is our passion and focus
REFERENCES & RESOURCES
- MedicalXpress, 2023. Study finds rural residents have 19% higher risk of heart failure than their urban counterparts. [online] Available at: https://medicalxpress.com/news/2023-01-rural-residents-higher-heart-failure.html
- American Heart Association, 2023. New efforts to improve cardiovascular, stroke care in rural areas. [online] Available at: https://newsroom.heart.org/news/new-efforts-to-improve-cardiovascular-stroke-care-in-rural-areas
- Centers for Disease Control and Prevention: Interactive Atlas of Cardiovascular Disease and Stroke Tables https://nccd.cdc.gov/DHDSPAtlas/Reports.aspx
- Centers for Disease Control and Prevention: Cardiovascular Disease Death Rates, 2014-2016; Adults, Age 35+, by County https://www.cdc.gov/dhdsp/data_statistics/fact_sheets/fs_heart_disease.htm
- Centers for Disease Control and Prevention: Cardiovascular Disease and Stroke Prevention – State and Local Public Health Action Programs https://www.cdc.gov/dhdsp/programs/spha/index.htm
- Intechopen.com: Strategies for Cardiovascular Disease Prevention in Rural Southern African American Communities; Ralphenia D. Pace, Norma L. Dawkins and Melissa Johnson; 2012 http://cdn.intechopen.com/pdfs/36934.pdf
- National Institute of Health: Clinical Utility of a Novel Coronary Heart Disease Risk-Assessment Test to Further Classify Intermediate-Risk Patients https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4231217/
- Rural Health Information Hub: Chronic Disease in Rural America https://www.ruralhealthinfo.org/topics/chronic-disease
- U.S. Department of Health and Human Services: Million Hearts https://millionhearts.hhs.gov/
By : AB Med Healthcare Solutions