Even though it is far from over, the COVID-19 pandemic has already left a deep and long-lasting imprint on healthcare facilities. Hospitals and their staff have taken the brunt of the COVID-19 healthcare onslaught with many being overwhelmed by patient numbers, particularly during surges. A comprehensive HHS report from March 2021 found that hospital administrators described the difficulty of caring for COVID-19 patients while trying to resume necessary non-COVID-19 operations [i]. Lack of resources, staffing shortages, facility limitations, and inadequate pandemic training were cited as the biggest issues leading to serious concerns for patient safety. The report went on to state that “hospitals reported that public trust in hospital safety and credibility has eroded during the pandemic.”
It’s clear that prioritizing patient safety and building up trust and credibility in your healthcare facility is critical at this point in the pandemic. There are many benefits to pursuing a safety-first environment. When safety incidents go down, costs also go down. Further, prioritizing safety increases employee morale and focus, which improves retention rates. The patient experience gets better, and their satisfaction improves.
Safety Training
The COVID-19 pandemic has made the importance of proactive safety measures even more apparent. Given the speed of transmission, precautions that manage outbreaks before they happen are crucial. But doing so requires comprehensive safety protocols that address and mitigate risk for your team. It also requires planning for an outbreak before it happens, putting procedures in place that will let your team mobilize quickly in situations where time is critical..
While it can be easy to take a reactive approach—solving problems as they come up—the cost in time, money, and possibly lives will be higher. You will never regret taking the time to step back and reevaluate how prepared you are in terms of preventative and responsive measures.
Below are some tips on how to put a safety and health management system in place that works to reduce risks, prevent accidents, and protect patients as well as all workers connected with your health care facility.
Healthy Communities, Healthy Facilities
Health care facilities that make safety a top priority prevent or reduce hazards and realize many benefits. Prioritizing safety allows employees to focus on their work. Accidents are prevented, and employee retention rates increase. Costs go down, and patient satisfaction goes up.
The COVID-19 pandemic has made the importance of proactive safety precautions even more clear. Given the speed of transmission, precautions that manage outbreaks before they happen are absolutely crucial, but doing so requires comprehensive safety precautions that address and mitigate risk for your team. It also requires planning for an outbreak before it happens, putting procedures in place that will let your team mobilize quickly in situations where time is of critical importance.
While it can be easy to take a reactive approach—solving problems as they come up—taking a moment to step back and reevaluate how prepared you really are in terms of preventative and responsive procedures and precautions is a must for all healthcare providers as society continues to navigate COVID-19.
While it can be easy to take a reactive approach—solving problems as they come up—taking a moment to step back and reevaluate how prepared you really are in terms of preventative and responsive procedures and precautions is a must for all healthcare providers as society continues to navigate COVID-19.
Below are some tips on how to put a safety and health management system in place that works to reduce risks, prevent accidents and protect patients as well as all workers connected with your health care facility.
Desire
The most important element in improving the safety of the work environment is the desire to act. There is a direct correlation between an institution’s strong commitment to safety and safe work behaviors. It is important to establish a “Culture of Safety” [ii] .
Take the Lead
The attitudes held by top-level staff affect everyone connected with a health care facility. According to an article published in “Becker’s Hospital Review [iii], there can be as many as 38 executives serving in top-level positions. They comprise the hospital or other health care facility’s “C-suite.”
Active leadership involves implementing the process, reaching for help if needed, listening to employee concerns, providing guidance and encouragement, taking steps to reduce hazards and setting a good example. As managers, what we ourselves do tells everyone around us whether we truly believe in the policies we set. If we routinely follow safety measures, others will too.
Get the Workforce Involved
Involving every employee in the planning process is vital to the success of any system meant to manage safety and health. Whether individuals work as a nurse’s aide, receptionist, cook, physician or janitor, they have knowledge, experience and concerns that are of value in planning. Each person knows something regarding safety that others do not.
The breadth and scope of the standards, policies and procedures that result from this input makes the system meaningful. Also, when we, as managers, involve every worker, we let them know that they are valued. Then, we must show that we mean it by following through, making changes where needed and doing everything we can to protect our employees.
An important part in all this is to provide ways for our employees to report problems. They must be allowed to request action for infractions that jeopardize their health and safety or the health and safety of others, including patients. We managers need to be ready to listen and to act in a manner that demonstrates that we hold our employees in high esteem and consider their safety, health and well-being a top priority.
Identify and Evaluate Hazards
Employees often see hazards before managers do. However, many times they do not understand the risk or know what action to take. Worker surveys and interviews, informal conversations, impartial assessments by third parties, and walk-around inspections by managers help spot hazards that otherwise may go unnoticed. A review of published materials regarding hazards common to the health care field also is useful.
Each facility is different. A careful evaluation of the most frequent types, locations and reasons of injuries will allow for a more targeted approach. OSHA has developed the 300 log [iv] to assist employers in cataloging injuries and illnesses. Review of the OSHA’s 300 log, will allow patterns to emerge and aid the administration with prioritizing their safety initiatives.
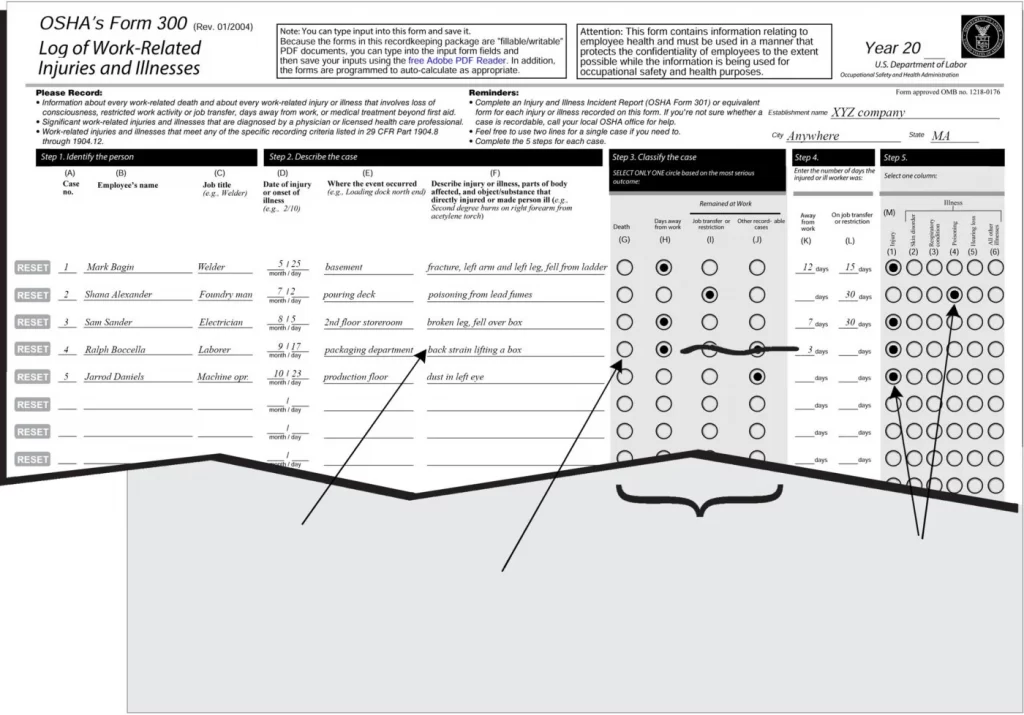
Once a hazard is identified, its ability to cause harm must be assessed. Good managers consider the worst possible outcome as well as the likelihood of that outcome. They think about who is at risk so that they can implement measures to reduce the risk. Brainstorming with employees who work around a given hazard can result in solutions that otherwise might not come to mind.
Prevent Hazards and Control Risks
Hazards in the health care field abound. Some can be prevented. Others must be controlled in order to keep workers and patients safe. At times, safety measures to prevent or control hazards are expensive. Yet, none are so costly that they are worth an employee’s life or the expense of paying for long-term illness or injury.
Here are several hazards that may jeopardize an employee’s safety, health or well-being:
- Exposure to chemicals
- Workplace violence
- Employee harassment
- Fatigue
- Uncontrolled access to medicines and supplies
- Lifting or moving patients alone
- Needle punctures
- Exposure to germs
- Poor lighting
- Machines that produce radiation
- Extreme noise
- Poorly designed rooms
- Slippery floors
- Inadequate protective gear
Educate and Train all Employees
Bureau of Labor statistics show that working in a hospital is more hazardous than working in construction. To provide worker safety in hospitals, we must provide education and training. Occupational health and safety improves greatly when all employees know how to protect themselves while at work. Fully trained workers make fewer errors. From emergency room procedures to how to prepare and serve a meal, worker education reduces harmful incidents that result from unsafe practices.
A common practice in construction is to hold “tailgate” safety training sessions. These sessions, also known as “toolbox talks,” are conducted at the job site at least once a week for no more than 20 minutes at a time. They cover work-specific safety information the attendees need to know in order to do their work safely and reduce risks. Tailgate training groups are small, presentations are informal, workers are allowed to ask questions, and only one topic is covered at a time. Training attendance is documented.
Even something as simple as how to put on and take off protective gloves requires training and practice in order for the safety measure to be routinely followed. As managers, we might be wise to make use of training sessions that follow the same guidelines as those observed in tailgate sessions. In addition, refresher courses and safety training for all new employees and for personnel who transfer to a new position need to be a part of the overall system.
Evaluate and Improve the System
In order for a safety and health management system to remain effective in ensuring worker safety in hospitals, every aspect of the system needs to be periodically reviewed and evaluated. Because the world of health care is constantly changing, older hazards may no longer pose threats while new hazards become commonplace.
Effectiveness of each policy related to occupational health and safety must be measured in order to determine what improvements need to be made. The hospital’s policy regarding the use of protective equipment such as sterile gowns and gloves only works as well as it is implemented by workers. It does no good to have a policy for reporting safety infractions if confidentiality is not maintained and no action is taken to prevent a second infraction.
Lack of awareness as to safety rules, policies and procedures causes many accidents and incidents. Lack of caring by top management adds apathy. Improving worker safety in hospitals requires every employee to be well informed and to truly care about their own safety and that of others. Let’s Connect.
The self assessment quiz below lets you check in on how your facility measures up to industry standards for safety. It offers an anonymous evaluation of your current safety precautions and procedures, offering feedback on where you might need to improve your existing policy in order to put safety first.
COVID-19 Disclaimer
At AB Med, accuracy is our highest priority, and everything we publish is up-to-date based on research and news at the time of release. However, due to the continually evolving nature of COVID-19, we are aware that available data changes quickly. The available data and recommendations may have changed since this article’s publication. Please check the CDC, WHO, and your local health department for the most current recommendations and news.
We at AB Med are excited to talk to you, Contact us
REFERENCES & RESOURCES
- Grimm, C. (2021). Office of Inspector General Hospitals Reported That the COVID-19 Pandemic Has Significantly Strained Health Care Delivery Results of a National Pulse Survey. [online] . Available at: https://oig.hhs.gov/oei/reports/OEI-09-21-00140.pdf.
- www.osha.gov. (n.d.). Healthcare – Overview | Occupational Safety and Health Administration. [online] Available at: http://www.osha.gov/SLTC/healthcarefacilities/safetyculture.html [Accessed 8 Sep. 2021].
- www.beckershospitalreview.com. (n.d.). 38 hospital and health system C-level roles, defined. [online] Available at: https://www.beckershospitalreview.com/hospital-management-administration/38-hospital-and-health-system-c-suite-executive-positions.html.
- www.osha.gov. (n.d.). Recordkeeping – Recordkeeping Forms | Occupational Safety and Health Administration. [online] Available at: http://www.osha.gov/recordkeeping/RKforms.html [Accessed 8 Sep. 2021].
By: Erik McLaughlin MD, MPH and Aikaterini Papadopoulou, B.Arch