The global pandemic of the SARS-CoV-2 virus and subsequent disease it causes, COVID19 is going to likely be the greatest medical challenge we have faced in the last 30 years. This guide is written by doctors, for doctors. We are the front line and must ensure we have good sharing of information, data, treatment strategies and emotional support. Quite simply, this is what we do and we are needed now, more than ever. Let’s work together, take a deep breath and follow evidence-based medicine.
Individual facility guidelines, state health departments and local input should always guide your practice of medicine. These are your primary sources of information. Within this article are broad swaths of information, a look at emerging treatment strategies shared from around the globe, guides for triaging patients, moving patients through your facilities and concerns for the future.This is not meant as a treatment protocol and clinicians should follow their institutional guidelines.
I encourage all of us to “run quickly but don’t run with panic”.
VIRUS BASICS
This virus was unknown until approximately 90 days ago. Much is being learned each day and much more is required before we begin to have hard guidelines. This section is meant to give some background on what is known and currently debated at the time of writing.
- The name of the virus is “SARS-CoV-2 and the disease caused by it is COVID-19
- From the Coronavirus family and related to MERS-CoV and SARS CoV
- Frequently reported signs and symptoms include fever (83–98%), cough (46%–82%), myalgia or fatigue (11–44%), and shortness of breath (31%) at illness onset[i]
- Spread via respiratory droplets in the air and from touching contaminated surfaces
- Incubation period of 2-14 days is current most accurate data
- Developing and distributing a reliable test has been a struggle
- At present, treatment is largely supportive care (fever control, hydration and rest)
- Patients with a mild clinical presentation may not initially require hospitalization. Clinical signs and symptoms may worsen with progression to lower respiratory tract disease in the second week of illness
- Deaths associated with COVID-19 are most commonly from Adult Respiratory Distress Syndrome (ARDS) and sepsis
- Data from Italy looks at 10% of all positive patients requiring Intensive Care (ICU) Support[ii]
- Elderly patients and medically fragile people appear to have the greatest risk of complications and mortality
- The current best protection is to avoid sick people, wash your hands, avoid touching your face, eyes, nose and mouth and to cover your cough and sneeze
- Clean frequently touched surfaces with commercial household cleaning solutions
- Surgical masks are for those already with symptoms and not required for uninfected people in the general population.
- Healthcare workers should adhere to strict contact, airborne and eye protection precautions
- Vaccine development is currently underway
- Treatment medications, antivirals and patient care protocols are being developed and studied
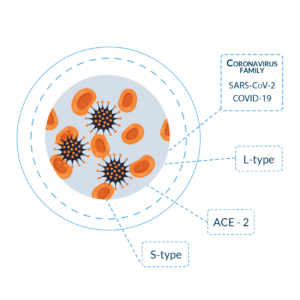
VIRUS FAMILY AND GENEALOGY
This virus was unknown until approximately 90 days ago. Much is being learned each day and much more is required before we begin to have hard guidelines. This section is meant to give some background on what is known and currently debated at the time of writing.
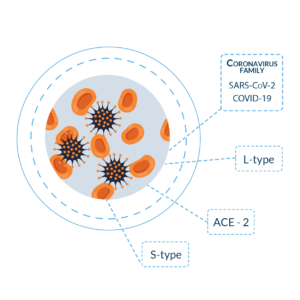
- Newly recognized nomenclature is the name of the virus is “SARS-CoV-2 and the disease caused by it is COVID-19”.[iii]
- Non-segmented RNA virus
- Non-segmented RNA virus
- Binds via ACE-2 (angiotensin converting enzyme 2) found on Type II alveolar cells and intestinal tissue [iv]
- Same receptor used by SARS
- Viral respiratory illness from the Coronavirus family
- COV19 is previously unrecognized in humans [v]
- Spread from human to human via respiratory droplets or contact with infected surfaces
- Symptoms can appear 2-14 days after exposure [vi]
- Limited reports show an incubation period of up to 27 days [vii]
- Reports are emerging of two related but separate strains of SARS-CoV-2 [viii]
- The concept of two strains is current being debated and investigated
- “L-type”
- Dominant strain in early days of the Wuhan outbreak
- Now not as common, globally
- Believed to have evolved from S-type
- Dominant strain in early days of the Wuhan outbreak
- “S-type”
- More commonly seen globally as pandemic spreads
- More closely resembles coronavirus from bats and pangolins
- May have been circulating for a longer period than known
SIGNS AND SYMPTOMS
Perhaps the biggest takeaway here is that patients begin developing worsening symptoms approximately 8 days into their disease progression. Deterioration can be rapid. Indications are that COVID19 lacks the typical runny nose and nasal congestion that seasonal influenza demonstrates.
- Common symptoms include fever, cough and shortness of breath[ix]
- Frequently reported signs and symptoms include fever (83–98%), cough (46%–82%), myalgia or fatigue (11–44%), and shortness of breath (31%) at illness onset[x]
- Fevers are considered a temperature greater than 38 C or 100.4 F
- Radiology exam with Chest CT scans shows 78% of known cases with either ground-glass appearance and/or consolidation on imaging [xi]
- Cause of death due to CoVID-19 is typically from Acute respiratory Distress Syndrome (ARDS) and sepsis11
- In one report, among patients with confirmed COVID-19 and pneumonia, just over half of patients developed dyspnea a median of 8 days after illness onset11
- Clinical signs and symptoms may worsen with progression to lower respiratory tract disease in the second week of illness11
- Data from Italy indicates 10% of all positive patients require intensive care unit (ICU) support[xii]
STAGES OF ILLNESS
As the patient beings to produce their immune response to the virus, approximately 6-9 days into the illness, the “cytokine storm” is believed to be the reason for the ARDS type picture and rapid deterioration.

- Replicative stage[xiii]
- Viral replication occurs over several days. Host immune response fails to contain the virus and relatively mild symptoms may occur
- Adaptive immunity stage
- As a stronger immune response begins to work, titers of the virus begin to fall. However, this also may lead to increased levels of inflammatory cytokines and subsequent tissue damage.
- This is the proposed explanation for patients are relatively stable for several days only to suddenly deteriorate when they enter this stage [xiv]
- Understand these stages are important for the following reasons[xv]
- Initial symptoms do not predict possibility for future deterioration
- Risk stratification will become increasingly important
- Early antiviral therapy will likely play a more important role during the early replicative stage
- Low dose steroids (immunosuppressive therapy) could be initiated during the adaptive immune stage to try and blunt the overwhelming immune response. (speculative)
TREATMENT GUIDELINES
These guidelines are a mix of recommended guidelines, current clinical trials and social media sharing between physicians, globally. Check with your institution for their protocol and current strategies.

- Current guidelines are based off February 11, 2020 CDC guidelines [xvi]
- Hospitalized patients should be treated in an Airborne Infection Isolation Room (AIIR) with standard contact, airborne and eye protection precautions
- At present, treatment is largely supportive care for non-ICU level cases
- Fever control with antipyretics such as acetaminophen and ibuprofen
- Hydration either oral or Intravenous (IV) routes
- Respiratory support up to intubation and mechanical ventilation
- There are current studies underway for antiviral medications (see below)
- Patients with a mild clinical presentation may not initially require hospitalization. Clinical signs and symptoms may worsen with progression to lower respiratory tract disease in the second week of illness[xvii]
- Possible risk factors for progressing to severe illness may include, but are not limited to, older age, and underlying chronic medical conditions such as lung disease, cancer, heart failure, cerebrovascular disease, renal disease, liver disease, diabetes, immunocompromising conditions, and pregnancy[17]
- In another report, the mean time from illness onset to hospital admission with pneumonia was 9 days[17]
- 20% of infected patients require hospitalization17
- 20-32% of hospitalized patients require ICU level support for respiratory problems[17]
- Acute respiratory distress syndrome (ARDS) developed in 17–29% of hospitalized patients, and secondary infection developed in 10%.[17]
- Cytokine Storm concept
- Similar to features of bacterial sepsis or hemophagocytic lymphohistocytosis (HLH)[xviii]
- Clinical features can be tracked with C-reactive protein (CRP) and ferretin
- Correlate with disease severity and mortality
- In one study, among critically ill patients admitted to an intensive care unit, 11% received high-flow oxygen therapy, 42% received noninvasive ventilation, and 47% received mechanical ventilation.[17]
- Some hospitalized patients have required advanced organ support with endotracheal intubation and mechanical ventilation (4–10%), and a small proportion have also been supported with extracorporeal membrane oxygenation (ECMO, 3–5%).[17]
- Other reported complications include acute cardiac injury, arrhythmia, shock, and acute kidney injury.[17]
- Prone ventilation for ICU/ventilated patients has been show as a promising adjunct[xix]
- Lower tidal volumes of 4-8mL/kg are being explored[xx]
- Lower inspiratory pressures (<30 cmH20) are also to be considered[xxi]
- Patients with moderate to severe ARDS should be considered to be treated with higher PEEP (positive expiratory end pressure)
- Avoid routine use of continual infusion of neuromuscular blockade agents
SPECIAL POPULATIONS
We are beginning to understand the “at-risk” population for COVID19 and know the elderly and medically fragile patients have the greatest concern. This section explores other special populations.

Children
- A recent study from China showed only 1% of infections were in children <9 years old[xxii]
- The same study showed only 1% of infections were in children 10-19 years old
- Mortality increases with age
- There have been no reported deaths in children less than 9 y/o
- Children 10-19 years old have a 0.2% fatality rate
- Schools in Japan have been closed for one month as of March 2nd through April 2020[xxiii]
- China and Hong Kong have also closed schools
Geriatrics
- Elderly patients appear to have the greatest risk of complications and mortality
- 50-59 y/o has 1.3% mortality
- 60-69 y/o has 3.6% mortality
- 70-79 y/o has 8% mortality
- 80 and above y/o has 14.8% mortality
- The US has a population aged over 65 of 49.2 million in 2016[xxiv]
- The US has 12.6 million people over the Age of 80[xxv]
Pregnancy[xxvi]
- Currently there is no published scientific reports about susceptibility of pregnant women to COVID-19
- Pregnant women experience immunologic and physiologic changes which might make them more susceptible to viral respiratory infections
- Pregnant women also might be at risk for severe illness, morbidity, or mortality compared to the general population as observed in cases of other related coronavirus infections
- There is currently no data on breastfeeding and communication of COVID-19 via breastmilk
- In limited studies on women with COVID-19 and another coronavirus infection, Severe Acute Respiratory Syndrome (SARS-CoV), the virus has not been detected in breast milk
INFECTION CONTROL AND PREVENTION
We all know how to limit infection spread. We need to be using our PPE, practicing good hygiene and taking extra precautions with aerosolizing procedures like intubations. Here is a synopsis on infection control and doing the best we can, at the moment.

The best way to prevent the virus is to avoid being exposed[xxvii]
- Stay away from sick people
- Avoid touching your eyes, noes and mouth
- Cover your cough and sneezes, throw tissues into the trash
- Clean frequently touched surfaces (door knobs, counter tops, banisters) with a common household cleaning spray or wipe.
- Handwashing with soap and water for 20 seconds or alcohol (60%) based hand sanitizers
- There are current efforts for vaccine creation and prophylactic medications (see below)
- The virus is spread via respiratory droplets from nose of mouth of infected people[xxviii]
- Droplets can land on surfaces
- Other people can touch these surfaces and infect themselves by touching their face, eyes, nose or mouth
- Healthy people in the general public have no benefit from wearing masks[xxix]
Infection control for healthcare workers[xxx]
- Take steps to ensure all persons with symptoms of suspected COVID-19 or other respiratory infection (e.g., fever, cough) adhere to respiratory hygiene and cough etiquette, hand hygiene, and triage procedures throughout the duration of the visit.
- Ensure that patients with symptoms of suspected COVID-19 or other respiratory infection (e.g., fever, cough) are not allowed to wait among other patients seeking care. Identify a separate, well-ventilated space that allows waiting patients to be separated by 6 or more feet, with easy access to respiratory hygiene supplies.
- Identify patients at risk for having COVID-19 infection before or immediately upon arrival to the healthcare facility.
- Inform infection prevention and control services, local and state public health authorities, and other healthcare facility staff as appropriate about the presence of a person under investigation for COVID-19
- Place a patient with known or suspected COVID-19 in an Airborne infection isolation room (AIIR) that has been constructed and maintained in accordance with current guidelines.
- AIIRs are single patient rooms at negative pressure relative to the surrounding areas, and with a minimum of 6 air changes per hour (12 air changes per hour are recommended for new construction or renovation). Air from these rooms should be exhausted directly to the outside or be filtered through a high-efficiency particulate air (HEPA) filter before recirculation. Room doors should be kept closed except when entering or leaving the room, and entry and exit should be minimized. Facilities should monitor and document the proper negative-pressure function of these rooms.
- If an AIIR is not available, patients who require hospitalization should be transferred as soon as is feasible to a facility where an AIIR is available. If the patient does not require hospitalization they can be discharged to home (in consultation with state or local public health authorities) if deemed medically and socially appropriate. Pending transfer or discharge, place a facemask on the patient and isolate him/her in an examination room with the door closed. Ideally, the patient should not be placed in any room where room exhaust is recirculated within the building without HEPA filtration.
- Once in an AIIR, the patient’s facemask may be removed. Limit transport and movement of the patient outside of the AIIR to medically-essential purposes. When not in an AIIR (e.g., during transport or if an AIIR is not available), patients should wear a facemask to contain secretions.
- Facilities should keep a log of all persons who care for or enter the rooms or care area of these patients.
Gloves
- Perform hand hygiene, then put on clean, non-sterile gloves upon entry into the patient room or care area. Change gloves if they become torn or heavily contaminated.
- Remove and discard gloves when leaving the patient room or care area, and immediately perform hand hygiene.
Gowns
- Put on a clean isolation gown upon entry into the patient room or area. Change the gown if it becomes soiled. Remove and discard the gown in a dedicated container for waste or linen before leaving the patient room or care area. Disposable gowns should be discarded after use. Cloth gowns should be laundered after each use.
Respiratory Protection
- Use respiratory protection (i.e., a respirator) that is at least as protective as a fit-tested NIOSH-certified disposable N95 filtering facepiece respirator before entry into the patient room or care area. See appendix for respirator definition.
- Disposable respirators should be removed and discarded after exiting the patient’s room or care area and closing the door. Perform hand hygiene after discarding the respirator.
- If reusable respirators (e.g., powered air purifying respirator/PAPR) are used, they must be cleaned and disinfected according to manufacturer’s reprocessing instructions prior to re-use.
- Respirator use must be in the context of a complete respiratory protection program in accordance with Occupational Safety and Health Administration (OSHA) Respiratory Protection standard (29 CFR 1910.134external icon). Staff should be medically cleared and fit-tested if using respirators with tight-fitting facepieces (e.g., a NIOSH-certified disposable N95) and trained in the proper use of respirators, safe removal and disposal, and medical contraindications to respirator use.
Eye Protection
- Put on eye protection (e.g., goggles, a disposable face shield that covers the front and sides of the face) upon entry to the patient room or care area. Remove eye protection before leaving the patient room or care area. Reusable eye protection (e.g., goggles) must be cleaned and disinfected according to manufacturer’s reprocessing instructions prior to re-use. Disposable eye protection should be discarded after use.
- Healthcare workers should revisit their procedures for donning, doffing and disposing their PPE[xxxi]
- Assume every person is potentially infected or colonized with a pathogen that could be transmitted in the health care setting.
- Strict contact, airborne and eye protection should be used for healthcare workers
EMERGING TREATMENTS
These concepts are currently being investigated and shared, globally, by treating doctors. These are medications to be familiar with and you could be seeing these pop-up on your individual protocols. Always follow your local guidelines.

- Chloroquine[xxxii]
- Antimalarial and autoimmune medicine
- Commonly found as an oral tablet
- Antiviral properties and immunomodulating effects
- Currently in FDA phase 3 study[xxxiii]
- 400mg by mouth, daily for 5 days
- One study appears to advocate a 1gm loading dose followed by 500mg BiD[xxxiv]
- There are questions on duration of treatment with this regime
- Remdesivir study[xxv]
- Oseltamivir
- Influenza A and B treatment
- Currently under investigation
- 75mg by mouth, twice per day for 5 days
- Ribavirin
- Hepatitis C antiviral treatment
- 1200mg twice per day
- Lopinavir/Ritonavir
- HIV antiviral treatment
- 400mg/100mg by mouth twice per day
- Brand name Kaletra
VACCINE DEVELOPMENT
- Multiple laboratories are working on vaccines
- Promising trials from Hong Kong[xxxviii]
- Moderna Theraputics from Massachusetts[xxxix]
- Novavax announced on 2/26/20 it has started testing COVID-19 vaccine candidates in animal models in the hopes of identifying a candidate to be used in human testing as early as this spring[xl]
COMMUNICABILITY AND TRANSMISSION
- R0 (R naught) is the basic reproduction number and predicts how many people one infected person spread the disease to another person[xli]
- R0 means the disease will likely die out on its own. One sick person usually does not infect another person, or less than one person.
- R1 means that one sick person infects at least one other person
- Measles has an R0 value of approximately 12-18 in unvaccinated people
- Seasonal influenza has an R0 of 1.2
- Smallpox R0 is 7
- SARS-CoV-2 has a R0 of 2.5
- There is concern for the ability to have a second infection after the initial infection has passed[xlii]

ARE YOU READY FOR COVID-19?
Assess your facility’s preparedness, take the test and find out if you are ready for COVID-19
Are you looking for a way to better prepare your rural facility for COVID-19? At AB Med Healthcare Solutions, we specialize in developing emergency preparedness solutions for rural healthcare facilities.
If you want to create a COVID-19 preparedness plan that is reassuring, accurate, and effective, contact AB Med today. Our experts are here to help!
The AB Med team is here for your facility and your community. We have the knowledge and experience to help you navigate through the challenges into a successful emergency plan Let’s Connect.
COVID-19 Disclaimer
At AB Med, accuracy is our highest priority, and everything we publish is up-to-date based on research and news at the time of release. However, due to the continually evolving nature of COVID-19, we are aware that available data changes quickly. The available data and recommendations may have changed since this article’s publication. Please check the CDC, WHO, and your local health department for the most current recommendations and news.
We at AB Med are excited to talk to you, Contact us
REFERENCES & RESOURCES
- Coronavirus Disease 2019, 2020, CDC, Center for Disease Control and Prevention https://www.cdc.gov/coronavirus/2019-ncov/index.html
- Hospital Preparedness Checklist, 2020, CDC, Center for Disease Control and Prevention https://www.cdc.gov/coronavirus/2019-ncov/hcp/hcp-hospital-checklist.html
- Masterson, L 2017, How Hospitals Can Prepare for an Influenza Pandemic, Healthcare Dive https://www.healthcaredive.com/news/how-hospitals-can-prepare-for-an-influenzapandemic/440696/
- Novel Coronavirus (2019-nCoV) and You, 2020, CDC, Center for Disease Control and Prevention https://www.cdc.gov/coronavirus/2019-ncov/downloads/hospital-preparedness-checklist.pdf
- EM-Crit COVID19 guidelines march 2, 2020
By: Erik McLaughlin MD, MPH and Aikaterini Papadopoulou, B.Arch






